
Static
By Marvin Tort
Late last year, the Department of Health warned that the number of Filipinos infected with Human Immunodeficiency Virus (HIV) might reach half a million by 2030 unless preventive measures and interventions significantly improve. Since 2020, the number of HIV cases in the Philippines has steadily risen.
If left untreated, HIV infection can progress to Acquired Immunodeficiency Syndrome (AIDS). HIV weakens the immune system, severely compromising an individual’s ability to combat infections and illnesses, including cancer. Timely and effective treatment is thus critical to prevent disease progression.
Current data indicate that HIV is now among the fastest-growing epidemics in the Asia-Pacific region. Locally, new HIV infections surged by 418% from 2010 to 2022, while HIV-related deaths increased by 535%. Additionally, average daily HIV diagnoses rose dramatically, from approximately nine cases per day in 2012 to as many as 57 cases daily by 2025.
According to the Joint United Nations Programme on HIV and AIDS (UNAIDS), key drivers of this epidemic include rising infections among men who have sex with men (MSM), particularly youth aged 15-24. UNAIDS data further highlight persistently low condom usage rates and insufficient funding allocated towards preventive programs.
Cultural and religious stigma also strongly discourages young individuals from regular HIV testing, leading to delayed diagnoses and treatment initiation. As a result, around 25% of newly diagnosed HIV cases are already at an advanced stage or AIDS upon detection.
In 2019, Congress enacted Republic Act 11166 or the Philippine HIV and AIDS Policy Act. Among its provisions, the law removed the requirement of parental consent for HIV testing among youth aged 15-17. It also mandated the expansion of HIV-related services across both public and private hospitals nationwide.
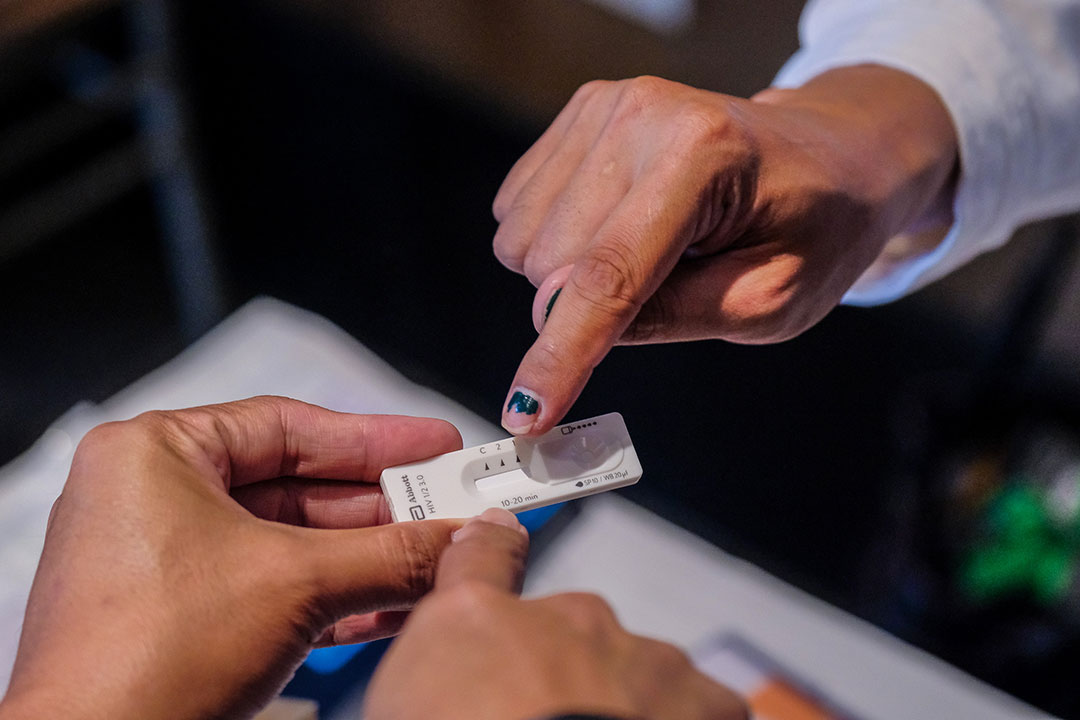
Despite policy advancements, the uptake of HIV self-testing (HIVST) remains low, mainly due to financial constraints. Self-testing allows individuals to use personal test kits conveniently at home. Yet, each test kit costs around P1,000, making it prohibitively expensive, particularly for low-income populations.
Similarly, Pre-Exposure Prophylaxis (PrEP), another critical preventive measure, remains inaccessible to many due to its cost. PrEP involves taking antiretroviral medication to significantly reduce the risk of acquiring HIV. When taken consistently, PrEP is said to effectively lower HIV infection risk by up to 99%. However, monthly costs for PrEP in the Philippines range from P1,500 to P3,500, a significant burden for many Filipinos.
Target groups for both HIVST and PrEP include individuals at high risk of infection: men who have sex with men, sexually active individuals with multiple partners or unknown HIV statuses, individuals in relationships with HIV-positive partners, and intravenous drug users sharing needles.
Globally, successful interventions exist. In Thailand and Australia, community-based testing, mobile testing units, and robust HIV self-testing programs reportedly increased early detection rates. Similarly, Brazil’s HIV prevention strategy focuses on widespread condom distribution coupled with comprehensive sexual health education programs, effectively reducing new infections.
To replicate these successes locally, the Philippine government and healthcare providers must broaden eligibility and access to PrEP through both public and private healthcare facilities. Moreover, comprehensive programs must actively encourage high-risk individuals to undergo regular testing and treatment.
The government could also enhance local outreach initiatives by improving viral load monitoring and drug resistance surveillance. This effort requires additional funding for laboratories to measure viral RNA levels accurately and detect HIV mutations that lead to drug resistance. Strengthening laboratory infrastructure and capacity remains crucial for effective HIV management.
Nonetheless, laboratory testing represents only part of the solution. The more challenging component is encouraging sexually active youth to engage in regular testing and treatment. Therefore, proactive public awareness campaigns and community outreach programs remain critical for increasing early diagnosis and timely treatment initiation.
Addressing preventive measures like HIV testing and medication accessibility remains complicated. Test kits’ high cost and prophylactic drugs’ expense pose considerable barriers. International aid or partnerships with pharmaceutical companies could significantly subsidize these costs, potentially enhancing uptake over the next five to 10 years.
Programs that substantially reduce or eliminate user costs can more effectively encourage people to test and seek preventive treatment. Generally, individuals seek to maintain their health and, if provided with affordable opportunities to test and receive preventive medication, they are likely to use them.
Providing free or subsidized testing kits and medications through government-run health centers and community programs represents a practical and achievable intervention. Yet, its success largely depends on health officials’ ability to secure sustained international aid and foster robust public-private partnerships.
Previously, a government-initiated, internationally funded condom distribution program significantly aided local HIV prevention efforts. In my opinion, correct and consistent condom use remains a highly cost-effective measure against HIV and other sexually transmitted infections, particularly crucial in rural areas and marginalized communities.
However, despite condoms’ proven effectiveness, free or subsidized condom distribution initiatives remain controversial within the predominantly Catholic Philippine context. Societal, religious, and cultural stigmas persist, limiting wider acceptance and consistent use.
Nevertheless, from a public health standpoint, condom distribution remains integral to comprehensive HIV prevention strategies. Ultimately, program success relies heavily on the government’s political will and commitment to addressing the HIV epidemic aggressively and systematically curbing viral transmission nationwide.
Marvin Tort is a former managing editor of BusinessWorld, and a former chairman of the Philippine Press Council